Iris Loew-Friedrich, CMO and Head of Development Solutions at UCB Shares her Thoughts on the Launch of New Innovators Campaign
Shots:
- Iris shared the specifics of the launch of the UCB’s Innovators campaign. The campaign spotlights the R&D employees’ perspectives on innovation and aims to highlight why innovation is a key driving force at UCB for bettering the lives of patients
- She gave her thoughts on how UCB is adopting innovative AI programs that use advanced analytics and algorithms to generate actionable outcomes from patient insights
- Through this interview, UCB’s focus on continuous innovation across all dimensions of research and development to solve the challenges in the lives of people living with severe diseases can be understood
Conversation with Iris Loew-Friedrich
Smriti: What led to the notion of improvements toward a more patient-centric approach to all aspects of R&D?
Iris Loew-Friedrich: Over the last decade, patients have been increasingly active and empowered when it comes to decisions concerning their health. Traditionally patients were viewed by pharmaceutical companies as simply users of our products, nowadays they are considered partners working towards a collective goal. As a result of this progression, our industry developed the notion of patient-centricity. At UCB we embraced this ‘patient centricity’ approach too but we believe it’s time now to move towards a true partnership with patients at every step of the pharma value chain, from R&D to manufacturing.
For UCB it’s no longer simply about validating assumptions or having patients participate in market research; instead, it has become far more valuable to co-create solutions with patients that tackle the diverse challenges that matter most to them as individuals and their caregivers.
In combination with data-driven insights generation, our multi-faceted approach toward truly understanding patient needs will enable our teams to design and execute development plans for products that effectively address unmet needs.
Smriti: Give our readers a brief detail about UCB’s Innovators campaign. Why did the company specifically decide to collect the perspective of its R&D employees?
“We are calling this our ‘Innovators’ campaign and it spotlights our R&D employees’ perspectives on innovation”
Iris Loew-Friedrich: For us, innovation is a concept that is constantly evolving and changing as new technologies, trends, research findings, and ideas emerge. But, most importantly, innovation needs highly skilled and motivated people to implement it. Because we know that our people are vital in the pursuit of innovation, and they are all unique, we set out to understand what innovation means to them and what they think makes a strong innovation culture.
We are calling this our ‘Innovators’ campaign and it spotlights our R&D employees' perspectives on innovation. Whether it is to bring new breakthroughs from lab to bedside or seeking to solve challenges for people living with severe diseases through collaborative partnerships, our campaign aims to showcase what drives innovation at UCB, how we approach innovation, and to celebrate our people, their talent, hard work and dedication to developing innovative solutions for the patients we serve.
Smriti: How does early direct patient and stakeholder input influence the overall R&D program strategy? What additional advantages does this provide?
Iris Loew-Friedrich: Based on a deep understanding of disease biology and patient needs, our research & development teams are conducting ground-breaking work to discover, develop and deliver highly differentiated medicines that we hope will transform treatment options and ultimately cure diseases.
However, we recognize that the solitary exploration of innovative ideas will never be as fruitful as it can be if we work together. We believe that the successful and sustainable company of the future will be the one in the middle of a ‘super network’ of partners, encompassing patients, academic centres, governments, and private companies, harnessing the latest breakthrough scientific discoveries into medicines that deliver real and relevant benefits to patients.
Our ‘super network’ approach challenges our thinking and exposes us to new ideas and ways of working, which is particularly important in the early stages of the R&D process. The patient voice at this stage helps us to ensure their needs are understood and embedded early in the research to help inform decisions, including the design and validation of specific patient-centered endpoints. It is a vital part of gaining a holistic and 360-degree, data-enabled view of a patient population and involves working together with all stakeholders to answer critical questions along the lifecycle of drug development. This is incredibly valuable as it means patient perspectives form the basis of future operations and outcomes.
Smriti: As you have mentioned about combining experimental data with artificial intelligence (AI), how has UCB used the latest advances in AI for creating an impact on drug discovery (any specific deals etc.)?
“At UCB we’ve been working closely with Microsoft to combine their computational services, cloud, and AI with our drug discovery and development capabilities.”
Iris Loew-Friedrich: Artificial intelligence (AI) in healthcare is an umbrella term to describe the use of ‘thinking’, or cognitive, technologies – such as algorithms, robotic process automation or machine learning. Put simply, AI is when computers and other machines mimic human cognition, and are capable of learning, thinking, and making decisions or taking actions.
It can be used to integrate patient experiences and opinions into solutions, further enhancing their value. In fact, AI can bring value to patients at almost every stage of the drug development and treatment process.
At UCB we’ve been working closely with Microsoft to combine their computational services, cloud, and AI with our drug discovery and development capabilities. Our biologists are now working side-by-side with data scientists to combine the data with computational methods – instead of manually collecting data, we are using Microsoft technology to create huge knowledge graphs in an unattended or automated manner.
One specific example is Research Canvas, where AI is applied to generate an overview of past and ongoing pivotal trials for a relevant indication, which is a notoriously complex activity from publicly available information. In addition, the user can extract the eligibility criteria and other relevant clinical, safety, and regulatory information. What would have taken weeks of human effort, can now be achieved in hours. We expect that Microsoft’s platform can support our scientists to discover new medicines in a more efficient and innovative way.
Using analytics and machine learning throughout the drug discovery, development, and innovation processes maximizes the value of data for patient outcomes. For example, developing state-of-the-art approaches to large data analytics, and combining AI with a Bayesian framework, better informs clinical trial patient selection and trial data analysis, as well as enhances logistics operations. At the clinical trial stage, AI can identify suitable cohorts by analyzing real-world data and social media content. Trial recruitment can be sped up by using AI technologies to alert medical staff and patients about trial opportunities, ultimately leading to more successful trials.
AI can play an important role in diagnosis, too. In 2021, we out-licensed Bonebot, now known as “Flamingo”, – an AI technology used to detect the presence of “silent” or asymptomatic fractures in the spine – to ImageBiopsy Lab. The technology will now be integrated into ImageBiopsy Lab’s existing hospital platform to increase reporting of vertebral fractures caused by underlying osteoporosis. AI can even spot malignant tumours invisible to the naked eye.
Smriti: How has working in close proximity with patients helped UCB deliver new and meaningful therapeutic options?
Iris Loew-Friedrich: Patients are increasingly active and empowered when it comes to decisions about their healthcare – they are no longer ‘users’, but partners and ‘co-creators’ in the R&D process. As the ultimate focus of everything we do, we work closely with patients to co-create solutions that put their needs at the centre.
UCB’s new robust end-to-end framework, designed to ensure that patients and key stakeholders provide direct input as early as possible into the overall strategy for research and development programs, will play a vital role in achieving successful outcomes for patient communities in the future.
One of the strongest examples of this is our Patient Engagement Council for Parkinson’s Research (PECPR), a partnership with Parkinson’s UK and the Parkinson’s Foundation to ensure that patient insights are central to the overall strategy and activities across UCB’s Parkinson’s disease research and early clinical development program. The council aims to embed patient involvement in the earliest stages and throughout each step of UCB’s Parkinson’s drug development programme.
The group’s focus includes decentralized research, the optimization of clinical trial design and experience, understanding disease modification therapy, and patient-informed Target Patient Value Profiles (TPVPs).
The purpose of a TPVP is to ensure that the drug development process provides all the required relevant medical, technical, and scientific information for evaluating the potential of a new medicine. Historically, the early design of TPVP’s was largely driven by joint insights from clinical scientists, desk research, and conversations with expert healthcare professionals, with little or no participation of people living with the condition.
Bringing patients into this process adds tremendous value, ensuring patient perspectives form the basis of our ambition for a certain molecule. In tandem, it provides an opportunity for patients to offer insights into unmet areas of need, outcomes that matter most to them, and potential areas of concern regarding study designs.
Smriti: Partnering with patients living with diseases being researched is indeed a great initiative. What impact does it have on the designing and implementation of clinical trials?
“We co-create protocols with patients / patient advocacy groups to help us to assess protocol complexity and minimize the patient burden”
Iris Loew-Friedrich: At UCB, our new framework centred around patients is designed to ensure that patients and key stakeholders provide direct input into the overall strategy for research and development programmes as early as possible, as well as the entire drug lifecycle. Clinical trials are a key topic for these interactions. Recruitment of patients into clinical trials is an ongoing challenge for all clinical studies. There is an opportunity to share more information about the benefits and need for clinical research and the many measures that protect patients’ safety and interests. Currently, only 5% of eligible patients participate in clinical research which illustrates the magnitude of the opportunity.
We co-create protocols with patients / patient advocacy groups to help us to assess protocol complexity and minimize the patient burden. An important element to minimize patient burden is the design of clinical trials in a way that minimizes interference with patients’ everyday lives. Bringing clinical studies to the patients’ home in the form of Decentralized Clinical Trials (DCT) and avoiding frequent visits to the clinic are building blocks for this approach. Today, approximately 46% of our trials have a DCT patient-centric component. DCTs make our clinical trials both more accessible and easier to participate in. They provide an alternative option for participation, helping us to reach patients in underrepresented geographies.
Smriti: Give our readers a brief detail about UCB’s recent formulation of FATIGUE- PRO to measure fatigue in Systemic Lupus Erythematosus patients.
Iris Loew-Friedrich: UCB recently constructed a new evidence-based approach to measure fatigue in Systemic Lupus Erythematosus (SLE), called FATIGUE- PRO (Patient Reported Outcomes) – developed in tandem with patients who described their direct and explicit experiences of living with the condition. Patients were concerned that many instruments used to measure fatigue come with limitations, such as not addressing the breadth of fatigue experienced. The research team collected qualitative data throughout the process, refining the parameters, including physical fatigue, cognitive fatigue, and susceptibility to fatigue, based on patient evidence.
The outcome was a new PRO instrument to measure fatigue that addresses the conceptional limitations of current tools, and that will have a significant impact on the lives of patients living with SLE.
The new patient-centred framework supports UCB’s scientists as they look to advance their understanding of human and disease biology. Listening and learning from patients at the earliest stages of research support a deeper appreciation of patients’ reality and unmet needs, allowing them to turn their scientific efforts towards pathways that may result in meaningful solutions that have the potential to transform the ways diseases are treated.
Smriti: Give us some more insight into your collaboration with the University of Southampton and the University of Bath along with the motive behind the collaboration.
Iris Loew-Friedrich: Collaboration is one of the most important steps toward innovation. We look for partners across disciplines who have a shared drive toward innovation in big, and sometimes small ways.
One of the most important (and smallest) examples of this is within our partnership with the University of Bath, where we partnered to produce miniaturised antibodies, potentially opening the way for a new class of treatments for diseases.
Until now, the smallest synthetic antibodies (known as monoclonal antibodies, or mAbs) have been derived from llamas, alpacas, and sharks, but the breakthrough molecules isolated from the immune cells of cows are up to five times smaller.
The potential medical implications of the new antibodies’ size are huge: From potentially binding to sites on pathogens that regular antibody molecules are too large to latch on to, triggering the destruction of invasive microbes, through to gaining access to sites of the body that larger antibodies can’t.
Our partnership with the University of Southampton allowed us to use our antibody expertise and innovative protein engineering to harness part of the human immune system known as the complement cascade to enhance the natural ability of therapeutic antibodies to attack blood cancer cells.
The new method was shown to be effective in several different antibodies. This makes it potentially attractive as a ‘plug-and-play’ modification tool to improve the performance of existing antibodies or create ‘bio-betters’ from existing therapeutics.
About the Author:

Iris Loew-Friedrich is the Chief Medical Officer for UCB, a member of the company’s Executive Committee, and Head of Development Solutions. She provides strategic global leadership for worldwide clinical development, medical affairs, regulatory affairs, quality assurance, statistical innovation, real-world evidence, and patient safety/pharmacovigilance. Her mission is to lead UCB’s Development Solutions, ensuring high quality, innovative, cost-effective development of objectively differentiated patient solutions with proven superior and sustainable value for clearly defined patient populations.
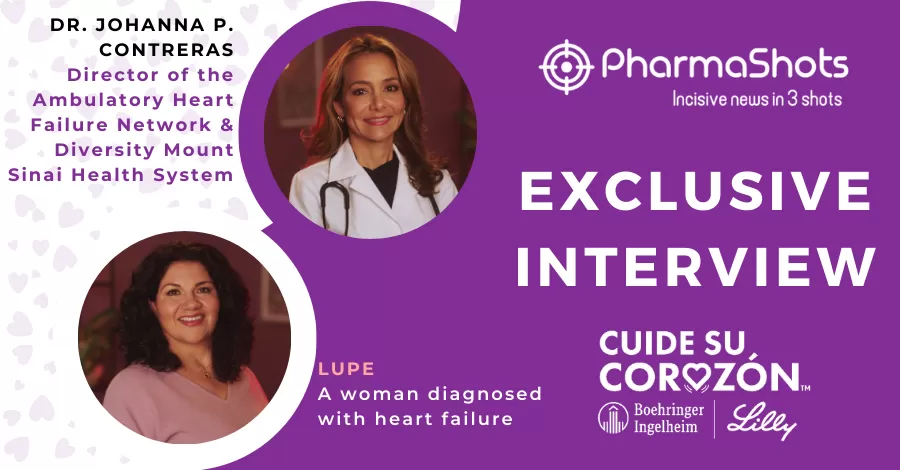
Related Post: Johanna Contreras and Lupe Share Insights from the Cuide Su Corazón Campaign
Tags

Senior Editor at PharmaShots. She is curious and very passionate about recent updates and developments in the life sciences industry. She covers Biopharma, MedTech, and Digital health segments along with different reports at PharmaShots.